The human body requires a plethora of nutrients for all of its systems to function properly on a cellular level. Most of the vitamins and minerals we require can be found in food, and typically, the best way to ensure you’re getting enough is to eat a well-rounded diet full of whole grains, fruits, vegetables, and lean protein sources.
The problem with eating healthily is that for many people, it’s just not feasible 100% of the time. Between busy lives and extensive options of delicious but not-so-great-for-you foods, it can be difficult to get all the nutrients you need through diet alone. This is why many people turn to supplements to help pick up the slack where their diet may be lacking.
While healthy people can benefit from most supplements if their body is low on certain things, those with chronic health issues such as autoimmune disease may not benefit from every supplement. In fact, some supplements can exacerbate certain conditions. If you have a chronic condition, you may be wondering, “What supplements should I avoid with autoimmune disease?” Read on to find out.
What is an autoimmune disease?
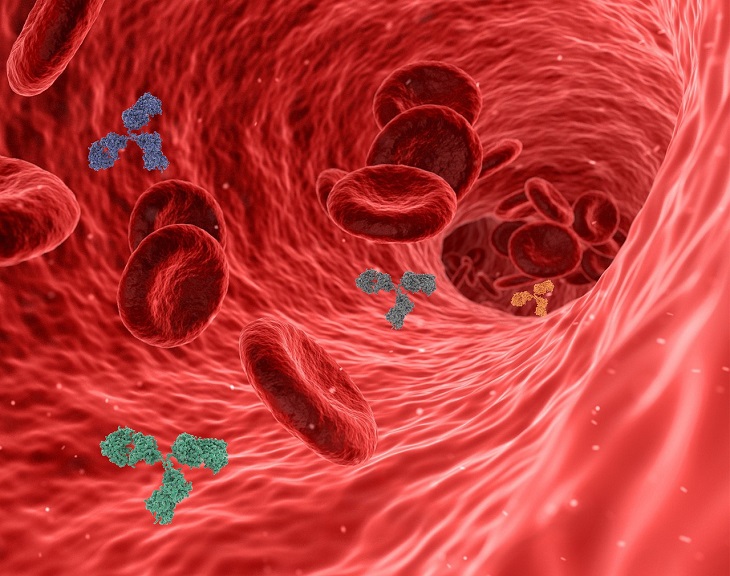
To understand what an autoimmune disease is, it’s important to understand how the immune system works. The immune system is the body’s first line of defense against pathogens and other foreign invaders that can cause illness. When a pathogen enters the body, immune cells spring into action in order to neutralize that threat.
A person with an autoimmune disease has a faulty immune system. Their immune response kicks into gear even when no threat is present and begins attacking the body’s own healthy cells, leading to cell damage. The cause of this reaction is unknown. Autoimmune diseases can affect any part of the body, and each type typically presents with its own symptoms and complications.

What can make an autoimmune disease worse?
As mentioned above, the exact cause of autoimmune disease isn’t yet known. However, there are a few factors that can actually increase the risk of a person developing one, or make the symptoms worse for people who do already have a type of autoimmune disease. Some things that can increase the risk of developing autoimmune disease include:
- Smoking
- Being related to someone with an autoimmune disease
- Having one autoimmune disease already
- Obesity
- Infections
According to research, one of the biggest factors that can affect the worsening of an autoimmune disease or a flare-up in symptoms is stress. Certain medications have also been shown to play a role in the exacerbation of symptoms.
Do vitamins make autoimmune disease worse?
Since the immune system is revved up and attacking the body’s own tissues in someone who has an autoimmune disease, it’s thought that anything that makes the immune response stronger could end up making the autoimmune disease itself worse. This includes certain vitamins.
According to a report in the Sun Sentinel, high doses of anything that will “rev up” the immune system (such as vitamin C, beta carotene, cat’s claw, or echinacea) may actually be more harmful than helpful for people with autoimmune disease. However, research into specific vitamins has harbored different results. For example, studies on the use of vitamin C as an addition to formal treatment for autoimmune disease has found that, although it shouldn’t be used on its own, it can actually help regulate the immune pathways within the body.
Herbal supplements, on the other hand, have been shown to be detrimental to people with certain autoimmune diseases. One older study published in 2004 looked at the use of echinacea and algae spirulina in people with autoimmune disease and found that the use of these supplements actually caused a flare-up in symptoms. Other studies have corroborated this evidence, such as one published in 2021 that looked at how herbal supplementation using spirulina, chlorella, echinacea, and alfalfa affected autoimmune skin diseases. The study also found flare-ups and an increased immune response after use of the supplements.
Despite these findings, the situation may not be so cut and dry. For example, one vitamin supplement could help someone with a specific type of autoimmune disease while making symptoms worse in another. That is why it’s also important to speak to your doctor prior to taking any new supplements. They will be able to tell you what would be best to take for your specific condition.

What supplements help autoimmune disease?
Research has been looking into certain vitamins and supplements that may be a welcome addition to a treatment plan for those with autoimmune disease, and has found that some vitamins could be helpful. One particular study examined the use of zinc and vitamin D in people with autoimmune disorders and found that these immune-regulating nutrients showed great promise in balancing immune function.
Other research has looked at supplements such as prebiotics and probiotics, fish oils, vitamin D, and curcumin as possible options when it comes to helping reduce disease flare-ups. The study found that each supplement could help in its own way when used to address a specific type of autoimmune disease. For example, prebiotics and probiotics may be helpful in treating inflammatory bowel disease; curcumin was also shown to be beneficial in people with ulcerative colitis, as well as rheumatoid arthritis.
These findings prove that, although supplements can help with autoimmune disease, the type of disease and supplement must be perfectly matched in order for the supplement to be a help rather than a hindrance.
Featured image by Towfiqu barbhuiya on Unsplash